This article is part of the systems administration guide. You will require administration access to view the pages mentioned in this article.
Contracts
For IHC, when translating an invoice into a claim, typically this is in the context of an agreement with a third party. This may be a Health Fund, it may be another entity such as DVA.
Depending on the specific item(s) being claimed from your invoice, you may need to map the specific terms and concepts from the invoice into a more general agreement.
For a health fund, the details of this are established typically in a pricing agreement directly with you, or via a legislative default.
The nature of contracts come in these broad categories:
- Which items can be claimed to a specific Health Fund.
- A fixed service code that needs to be used for that Health Fund.
- A derived service code based on other information in the admission that needs to be used for that health fund.
- The segment type that needs to be used for that Health Fund.
Definitions: Rate Contracts and Claim Contracts
Effective v6.63, existing contracts used to manage step downs for accommodation services will be called Rate Contracts. In addition, a new type of contract has been added called Claim Contracts.
Contract System Administration
Searching and Viewing Claim Contracts
- From the Contract interface, click the Claim Contracts tab.
- Click Change Search Criteria.
- The Search panel appears.
- Specify one or more search criteria, as needed.
- Default Search Filters: Global Contracts set to "False" and Billing Allowed is set to "Yes or No".
- In the Global Contracts field, select the checkbox to indicate that all global contracts should be included in the search (selected by default). If selected, then claim contracts with no item code will be included in the search results.
- In the Item Number field, select an item number from the drop-down list.
- In the Guarantor field, select a guarantor from the drop-down list.
- In the Service Location field, select a service location from the drop-down list.
- In the Rate Contract field, select a contract from the drop-down list.
- In the Billing Allowed field, select either Yes, No or Yes and No (default), as applicable.
- Note: CareRight automatically stores defined filtering options and applies them if no additional filtering criteria are specified.
- Click Create Search contract.


| Column Name | Description |
| Item | Item number linked to item view. |
| Guarantor | Guarantor code linked to guarantor view. |
| Service Location | Service location name linked to service location screen. |
| Rate Contract | Rate contract name linked to rate contract screen. |
| Service | Service type. |
| Strategy | Service code strategy. |
| Code | Service code. |
| Type | Service code type. |
| Program | Program code. |
| Bed Level | Bed level code. |
| Allowed | Is billing allowed? Yes or No. |
| Paper Claim | Send as paper-based claim? Yes or No. |
| Accom Warn | Warn if not billed with accommodation charge? Yes or No. |
Add New Claim Contract
- Click Administration.
- Select Accounting Menu item.
- Select Contracts sub-menu item.
- The Contracts screen will display with all the existing Items, if any.
- Select the New button.
How to Delete a Claim Contract
- Search for a claim contract.
- In a contract row, click Edit.
- In the Claim Contract panel, click Delete.
- A deletion confirmation windows appears.
- Click OK.

Add New Rate Contract
- Click Administration.
- Select Accounting Menu item.
- Select Contracts sub-menu item.
- The Contracts screen will display with all the existing Items, if any.
- Select the New button.
- The add new Contract screen will display.
- Enter the Name of the Contract.
- Select the relevant Item number from the drop-down list.
- The description will auto-populated.
- Select the Create Rate Contact button, this will return you to the Contracts list.
- Select the Show button next to the newly created contract.
- The Contracts detail will display, with the following sub-sections:
- Details - Name of contract
- Item - Item being charged and description.
- Rate Definitions - This is where you define which rate definition is to be used for the Contract Item billing.
- Grouped Contracts - Please contact Clintel for further information
- Unit Rules - This is where you set up your step date rules and rates for the item. Note: The Item must have the Stepped Service Date checkbox enabled in the Item settings
Claim Contracts Selection
Within CareRight, the claim contract configuration is minimal billing rules engine. Based on the details of the invoice/line item you are claiming, the system will search for the most specifically matching to least specific rules.
Claim Contracts are used to control what items can be claimed and the process around generating the correct claim. Rules are applied based on match criteria, called keys. An item can have multiple claim contracts which are presented in an order of priority. The first matching rule found for an item is the rule that is applied.
For example, you may wish to block all billing by adding only a global claim contract with billing disabled; and then add specific individual claim contracts with detailed mapping and billing enabled for combinations of:
- Item
- Guarantor
- Service Location
- Applicable Rate Contract
Contract Setup
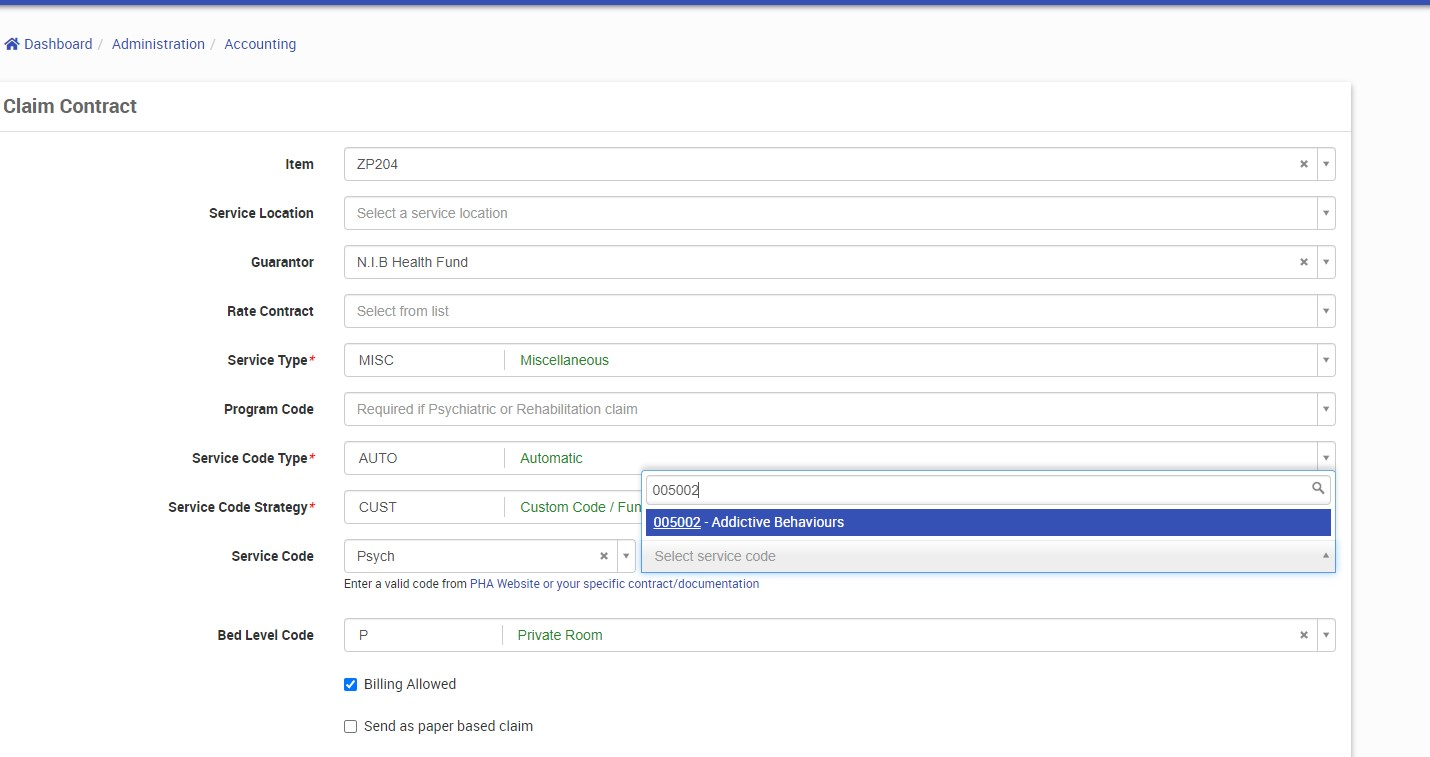
Parts of a Claim Contract
There are three areas of the Claim Contract, the first determines how the contract matches - Item, Service Location, Guarantor or Rate Contract.
Where an item is left blank, it matches everything.

The next section of a Claim Contract is about how the contract maps from your data. This includes a number of built in strategies, which assist in mapping the required information

The final section controls defaults and behaviour. For example, if you have a specific program or always use a Bed level code of Private, these can be specified.
Behaviour controls - if the item can be billed at all, if it requires a paper claim, or if it must have a corresponding accommodation charge can be indicated here.

- Send as paper based claim: Some health funds only support paper-based claims — this option supports that requirement; and,
- Warn if not billed with an accommodation charge: When an item is being added to the invoice, if the claim contract associated with the item has the checkbox "Warn if not billed with an accommodation charge" checked and the invoice does not have any items of type accommodation, then a warning will be displayed: "This item is expected to be billed with an accommodation charge. Verify with the health fund that this will be accepted or add an accommodation charge to the invoice."
Rules and Strategies for Mapping
Rules can apply the following behaviour:
Service Type (service_type): The service type can be set to:
- Auto (recommended)
It will be set based on the Item Type of the item.- "HCP Accom Charge" = "Accommodation"
- "HCP Theatre Charge" = "Theatre"
- "HCP Bundled Charge" = "Bundled"
- Any other type = "Miscellaneous"
Manually chosen options are useful when you need to override default behaviours.
- Accommodation
- Theatre
- Miscellaneous
- Bundled - Where you know a specific item is Bundled Accommodation and Theatre - sometimes known as a Case Payment.
Here the system will present additional options, if you need to specify different codes for the accommodation and theatre items.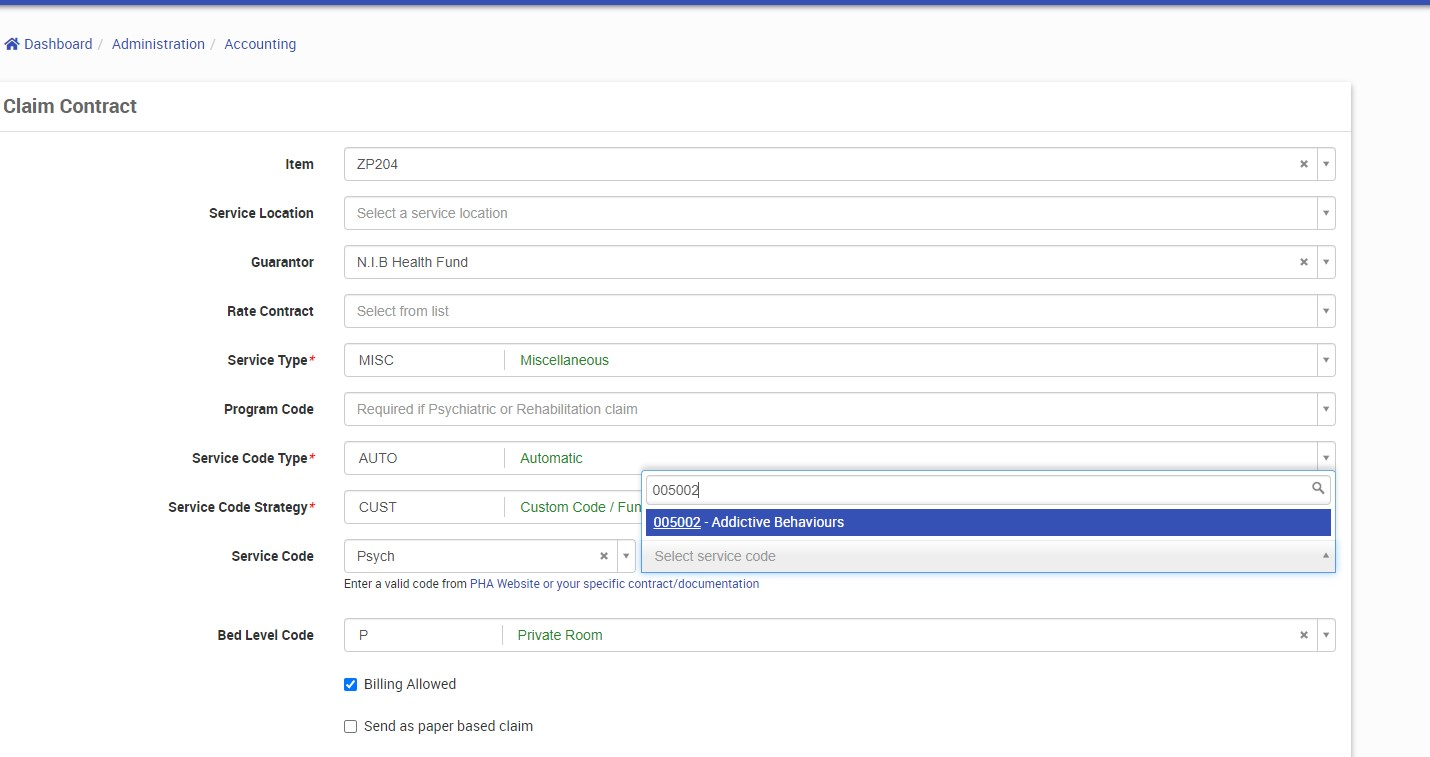
If set, these fields are used to populate the ACD segment instead of the existing service code and service code type fields. The existing Service Code and Service Code Type fields will continue to populate the SVB segment.
If the Bundled Accom Code field is blank and the Bundled Accom Type is set to "AUTO" then when populating the ACD segment the values from the Service Code and Service Code Type will be used. (As per current behaviour).
When creating a new Claim Contract the Bundled Accom Code will be blank and the Bundled Accom Type will be AUTO.
A migration will set all existing claim contracts to have a Bundled Accom Type of Service Code Type and Bundled Accom Code of Service Code.
Service Code Strategy
Note: Translated from format_service_code(item, admission).
- AUTO (recommended)
Breaks down the Item Number to attempt to resolve it to an MBS Item, Number of Patients Seen, and Assistance Item if relevant.
Examples:Item Number Mapping Explanation 13215 13215 13215_Case 13215 Only the numeric portion extracted, then processing stops W112 W112 As per above, however any prefixed characters are also extracted W112_Case W112 13215/4 13215
4 patients seenA slash between the item followed by a number indicates the number of patients seen 13215\4 13215
4 patients seen13215S 13215
Assistance Item: trueAppending an S indicates this is an assistance item. FAKE_NUMBER_HERE FAKE_NUMBER_HERE The system cannot recognise anything to extract, so passes this directly through unmodified. - MBS - As above. AUTO is an alias of this implementation.
- DIAG - Looks up the admission principal diagnosis code. Removes any non A-Za-z0-9 characters.
- DRG - Looks up the admission diagnosis related group. Removes any non A-Za-z0-9 characters.
- CUST - Returns the value entered in Service Code. Useful when there is not a standard, clear mapping.
Service Code Type (service_code_type)
Note: Translated from: format_line_item_service_code_type(line_item) to get the serv_cd_type.
Maps the service type code, usually by inspecting a specific line item (item), and guarantor within the context of an admission.
| Scenario | Output |
| DVA | V |
| MBS | C |
| DRG | D |
| ICD | I |
| MISC | M |
| PROS | P |
| OTHR | O |
| AUTO - service_code_strategy is DRG | D |
| AUTO - service_code_strategy is DIAG | I |
| AUTO - Item code is a PROSTHESIS_CHARGE | P |
| AUTO - Guarantor is DVA | V |
| AUTO - Formatted service code is numeric (MBS) | C |
| AUTO - Everything else | O |
Parts of a Rate Contract
Select Rate Definition
- Select the Edit button in the Rate Definitions section
- The available Rate Definitions will display with an available checkbox
- Enable the check box for the relevant Rate Definition.
- Select the Update Contract button
- Note: If the Rate Definition does not exist it will need to be created - see Rates Definition
To Add Unit Rules
- Select the New button in the Unit Rules section.
- The Contract Unit Prices screen will display.
- Add the following details:
- Units - this is the day which the price relates to (e.g., Day 1).
- Price - this is the chargeable amount for that day (e.g., $300.00).
- Description - this is a description of the Unit Rule - Day 1 rate.
- Service Code - Optional. Only provide if you wish to provide multiple step down types or rates for a given day range. Must relate to the Program Code.
- Program Code - Optional. Available Program Codes from the applicable Guarantors for this rate contract. Only provide if you wish to provide multiple step down types or rates for a given day range.
- The following is an example of a full Unit Rate set up, with multiple services catered for:
Units | Rate | Description | Service Code | Program Code |
1 | $300 | Day 1 Rate | PS00005014N | PS00005014O |
| 1 | $310 | Day 1 Rate | PS00005014M | PS00005014O |
2 | $250 | Days 2 & 3 Rate | PS00005014N | PS00005014O |
4 | $200 | Days 4 - 10 Rate | PS00005014N | PS00005014O |
11 | $150 | Day 11 onwards | PS00005014N | PS00005014O |
How do Program Codes appear?
In the UI, you are presented with available program codes:

Program Codes are available via the Guarantor, who is in turn associated with the Contract.
For example; if you had a Guarantor configured for BUPA Australia; you would add your admission program codes:
And that Guarantor would be added to a Rate Definition:
This would be associated then in turn with the Rate Contract

Rate Contract for Item Screen
Editing cannot be done from this screen. It must be done directly from the Rate Contract screen.

Datasets (since 6.65)
Name: ClaimContract
Table: claim_contracts
Association / Joins to other dataset tables
- Service Locations (via service_location_id)
- Guarantor (via guarantor_id)
Fields
- service_type
- service_code_strategy
- service_code
- service_code_type
- bundled_theatre_code
- bundled_theatre_type
- program_code
- bed_level_code
- billing_allowed
- send_paper_based
- accomodation_warning
Derived Fields
- item_number (item_id -> item.item_number) as a string
Not Supported in this iteration of the dataset
- Rate Contract