Statutory reporting is the mandatory submission of financial and non-financial information to a government agency. The health industry in Australia has its own set of laws and regulations that mandate the format and the data of statutory reporting.
CareRight supports each states legislation for submitting statutory reports:
- AAPC - ACT Admitted Patient Care Data Collection
- HCP - Hospital Casemix Protocol
- HMDS - Hospital Morbidity Data System
- ISAAC - Integrated South Australian Activity Collection
- PHISCo - Private Hospital Inpatient Statistic Collection
- QHAPDC - Queensland Hospital Admitted Patient Data Collection
- QLDCNR - Queensland Cancer Registry
- TAS - Tasmania Statewide Morbidity System
- VAED - Victorian Admitted Episodes Dataset
Statutory reporting is mandatory for all practices or specialists who deliver any type of surgery.
Reporting Criteria
The reports will generate days of admission based on each state requirements (i.e. taking into consideration if a patient has a leave day). Reports are also based on discharge date, not admission.
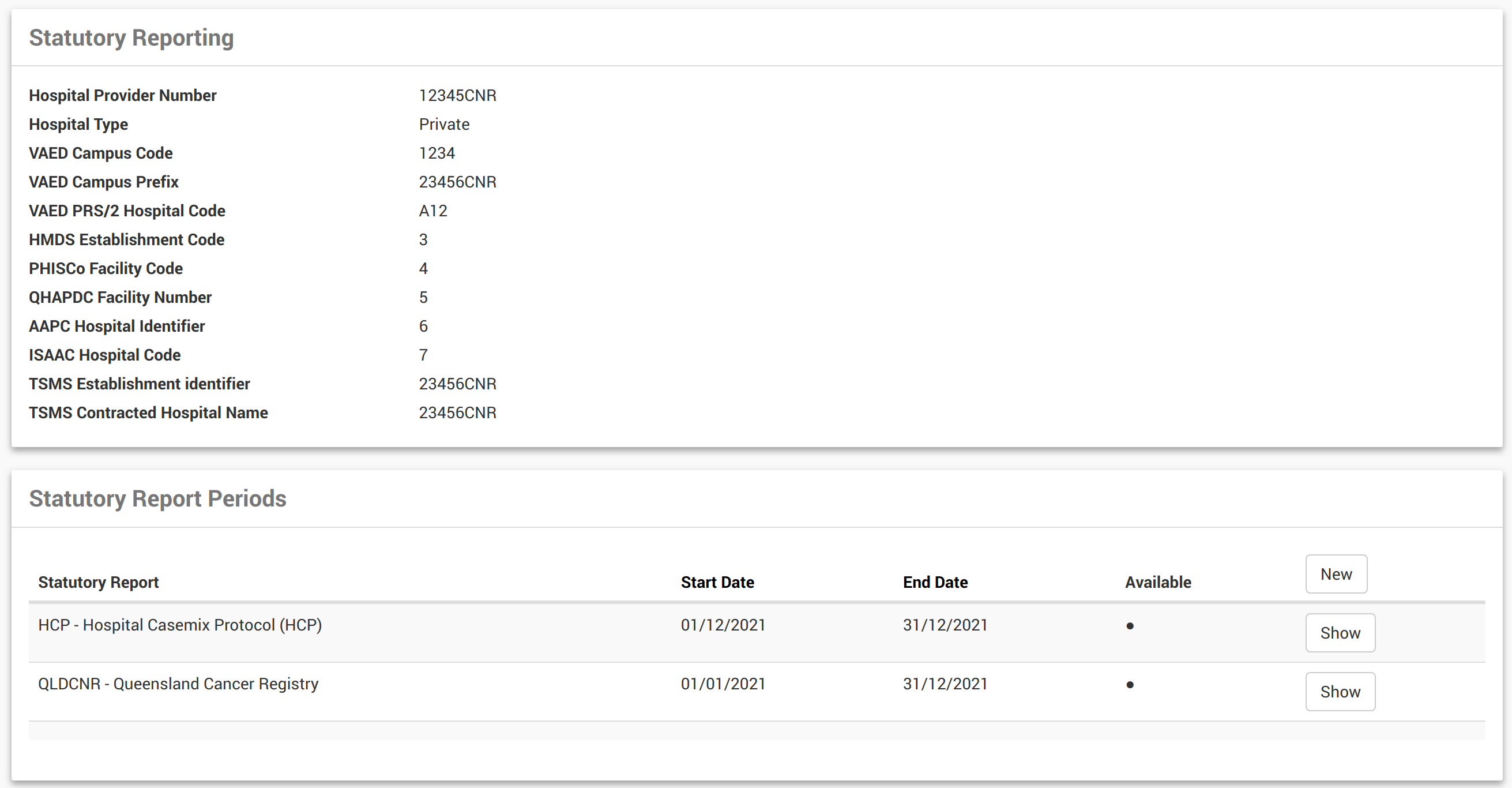
Initial Setup
Prior to running statutory reports, your System Administrator must complete a few steps:
- Create Locations which need to provide reports.
- Ensure each Location has a Hospital Provider Code and legislation code(s) defined.
- For System Administrators, to add a reporting period, System Administration > View location > Select New
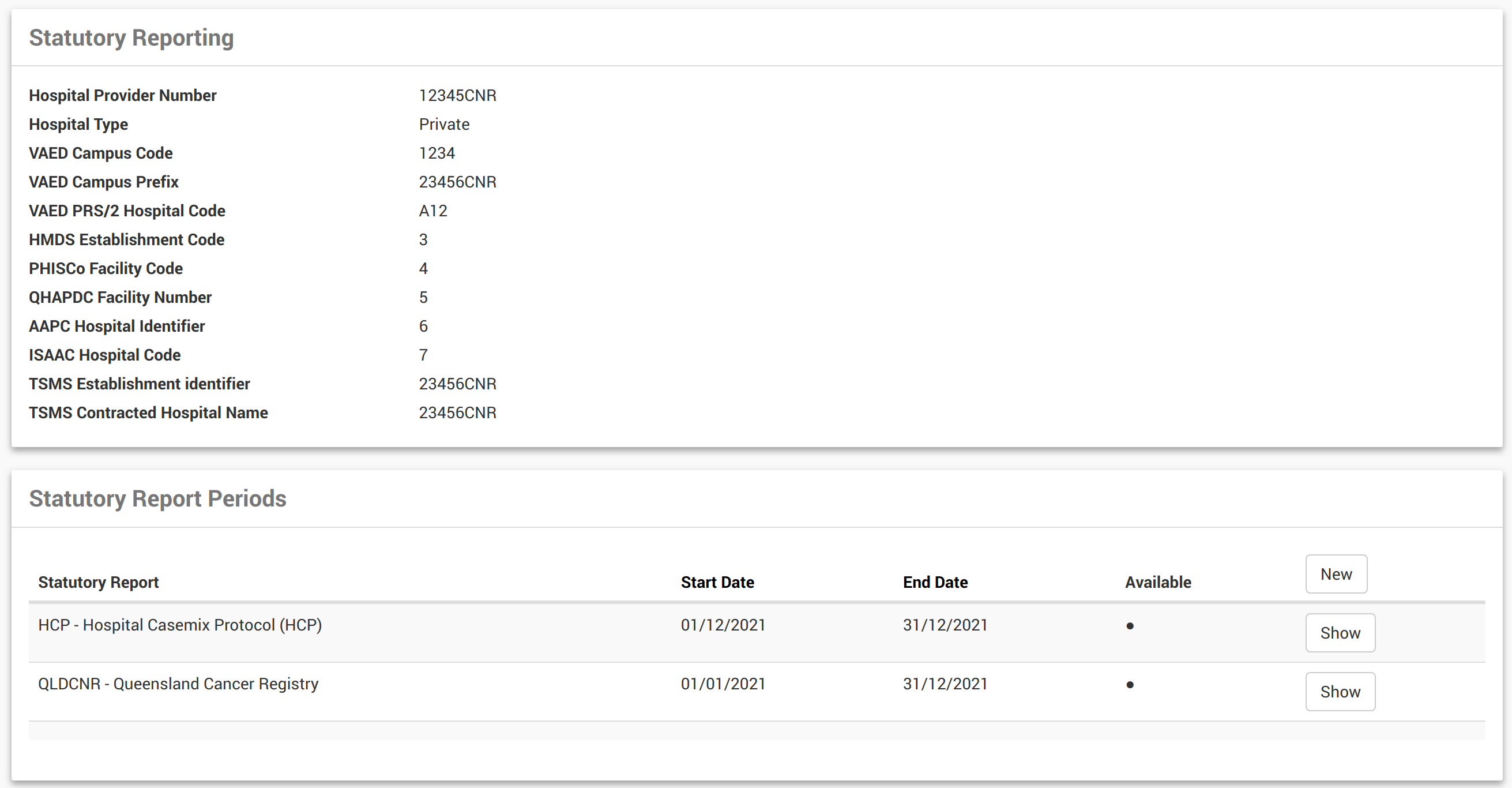
- For System Administrators, to add a reporting period, System Administration > View location > Select New
Permissions
Statutory Reporting and access permissions will be assigned by your System Administrator. Please refer any access queries to your System Administrator.
State Base Cancer Registry Reporting (Notifications)
CareRight has been configured to run Cancer Registry reports utilising the existing Statutory functionality - See Running Reports - Cancer Registry
Holding Admissions from Extract
These may be ‘admissions’ that we have a contract with the Health Fund and billed as Outpatient Medical Services (OMS). These are not usually admitted and therefore aren’t required to be reported to State Health. We have to admit and code these ‘admissions’ so that the Health Fund will pay. The Health Funds have advised that they do not require us to send these through HCP.
This is now supported by making an Outpatient admission.
- Set the same day status to Non-admitted. These are excluded from stat reporting.
- To claim you may need to set the optional field Service Category to 6 on the IHC claim form.
Gender Definitions
CareRight uses gender options that are aligned with standards established by the Australian institute of Health and Welfare. These are:
- Male
- Female
- Other
Consolidated Change Reporting for VAED Reports (v6.67.3 Enhancement)
The Victorian Department of Health and Human Services require that VAED monthly reports include changes to previous admissions, when applicable. In order to support this directive, CareRight now offers consolidated change reporting for VAED statutory reports.
Regenerating Reports
When regenerating reports, only the last month's report for that financial year will be available for regeneration. This means that the report for June for any year can always be regenerated and submitted to VAED, provided that it has met eligibility for its initial creation.
Note in the example below, the Regenerate button is hidden when there is a more recent report within the financial year, though June is still available for regeneration.

Include Entire Admission History
When the Include entire admission history for YTD checkbox is selected, then all admissions for that financial year up to the end of the current reporting month will be included in the VAED report, even if they have not been changed. By default, this option is unchecked.

Run individual fund HCP extracts (v6.69.3 Enhancement)
There are instances where hospitals may not be able to bill some admissions while negotiating health fund contracts, however. they still need to submit statutory reporting for those admissionons. Pre 6.69.3 is not capable of generating statutory reports if any of the fund's admission has no invoice.
6.69.3 Enables this feature where the following set of rules will be applied.
The following fields will be filled as $0
- HCP/PHDB > accommodation_charge
- HCP/PHDB > theatre_charge
- HCP/PHDB > labour_ward_charge
- HCP/PHDB > intensive_care_unit_charge
- HCP/PHDB > prosthesis_charge
- HCP/PHDB > pharmacy_charge
- HCP/PHDB > other_charges
- HCP/PHDB > bundled_charges
- HCP/PHDB > hospital_in_the_home_care_charges
- HCP/PHDB > special_care_nursery_charges
- HCP/PHDB > coronary_care_unit_charges
The funding source will be determined as follows:
If the admission has a pre-admission and the preadmission identifies the guarantor then that guarantor is used to determining the payer identifier.
If the admission has no pre-admission and the patient has health fund details recorded then assume the admission will be billed to that health fund and use that the payer identifier.
If the admission has no pre-admission and the patient has no health fund details recorded then assume the patient is paying and sen the payer identifier as self-insured.
The following report fields will use the determined funding source:
- HCP/PHDB > insurer_payer_identifier
- AAPC > funding_source
- HMDS > funding_source
- ISAAC > funding_source
- QHAPDC > funding_source
Invoicing Change
When creating an invoice that is linked to an admission ensure the admission is flagged for resubmission.
Note: Having no invoice no longer raises an error when generating stat reports and detail the rules described.