Generate an HC21 Form
HC21 claiming is a manual process to claim In-Hospital claims via the HC 21 Form. For some Health funds, this may be the only option while, for others, it may be an interim process whilst eclipse claim onboarding is occurring.
HC21 can be printed in two different ways from CareRight.
1. When completing the pre-admission steps for a patient also print the HC21 form from a patient record. This will complete all values on the left side of the form and you can have your patient sign it when they arrive. The right side can be printed later after the patient been discharged and a claim is generated.
2. Print both the Left and Right sides together at the end of the claiming process and the patient sign in it after the discharge/claiming.
CareRight can be configured to streamline the printing process that matched your business process.
Please refer to the Configurations for IHC Claims in system admin manual for more information.
Create an HC 21 Form
From the invoice eligible for IHC Claim,
- Click on the Claim Button
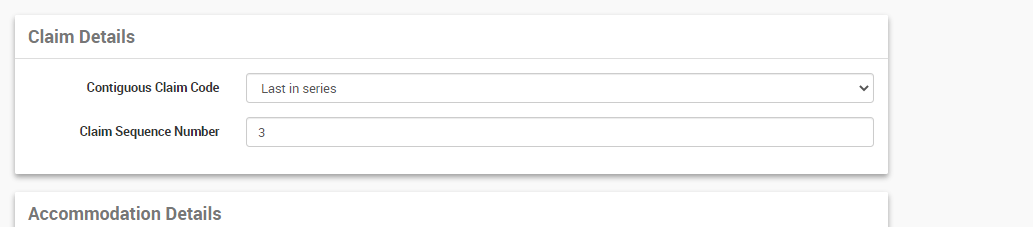
- The next tab will take information on the series levels the claim is submitting for and the sequence number if supplementary claims are submitting as part of the same admission.
- Eg: If multiple Claims are submitting as part of admission, each claim can be assigned with series levels. Clients can claim multiple invoices associated with an admission together or they can be sent individually. If sending individually, the user has to select the Contiguous Claim Code manually as;
- Not is series - If the claim is not part of a series of claims associated with the admission
- First in series - If it is the first claim for the admission and more claims to come on.
- Middle of series - any claims between first and last claims in an admission.
- Last in Series - If it is the last claim in the series for the admission.
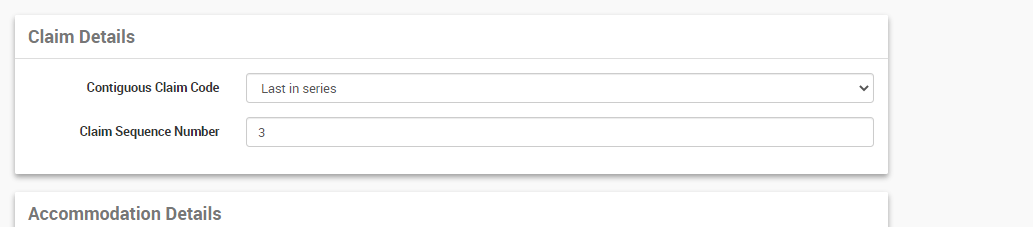
- The Claim Sequence Code will automatically be selected by the system.
- Eg: If multiple Claims are submitting as part of admission, each claim can be assigned with series levels. Clients can claim multiple invoices associated with an admission together or they can be sent individually. If sending individually, the user has to select the Contiguous Claim Code manually as;
- Click Next
- Review the information, Ensure all mandatory fields are filled.
- Any additional notes can be entered in the Remark text area, this will transfer as part of the claim.
- Any fields that have not been completed will give a red error message
- Click Prepare
- The HC21 Form can either be downloaded from the claim tab or Click Print HC21 from the invoice, based on the global settings
- If the user has global setting 'Embed Printed Billings' true and global setting 'Auto Print' true then display the invoice show screen and show the generated HC21 form in a popup dialog and auto print it.
- If the user has global setting 'Embed Printed Billings' true and global setting 'Auto Print' false then display the invoice show screen and show the generated HC21 form in a popup dialog.
- If the user has the global setting 'Embed Printed Billings' false then display the invoice show screen and trigger a download of the HC21 form.
 Download HC21 from the Claim
Download HC21 from the Claim
 Print HC21 from the Invoice
Print HC21 from the Invoice
If the system configured to print only the right side of HC21 and the user still needs to print both sides, this can be done in the View button either from Claim or from Invoice.
From this tab, user can either print
- The right half of HC21 Claim Form, or,
- Complete HC21 Claim Form


Claiming without DRG Code
For some facilities, it is possible to claim IHC paper-based claims without recording a DRG code. This can be configured in the admission category.
Please refer to Admission Categories in the System Admin Guide.