Eclipse Remittance Advice - IMC Claims
Eclipse Remittance Advice (ERA) will be provided by Medicare for all the IMC Claims.
ERA comprises of
- Processing Reports
- Payment Reports
CareRight is capable of automatic fetching of these two reports, however, this can also be reprocessed or fetched manually if the system fails to do so.
1. Processing Report
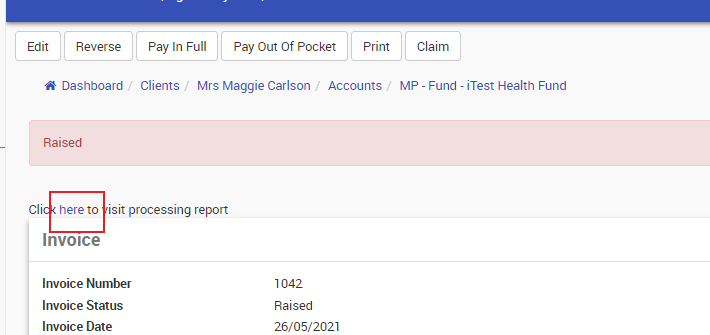
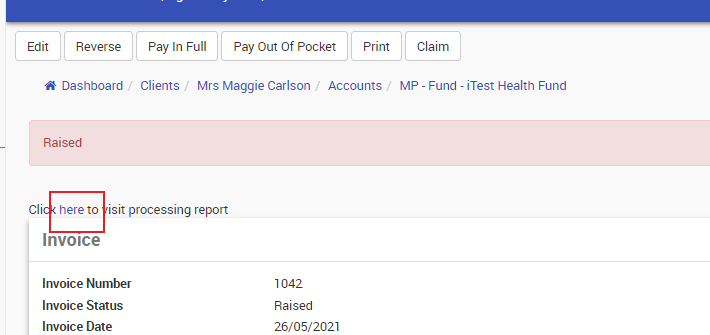
Processing Reports will be available within a day/couple of days after the IMC Claim is submitted. This can also be reprocessed manually via the Reprocess button available in the top left corner (Ref Fig 01).
This will provide the user an initial assessment output from Medicare. Also, the processing report will give information on how much the health fund and Medicare are going to pay for the claim.
 Fig 01
Fig 01
- Charged: The amount invoice been charged
- Medicare Paid: Contribution from Medicare
- Fund Paid: Contribution from the health fund.
- Scheduled fee: Total claim amount will receive (Medicare contribution + Health fund Contribution)
Accessing the Processing Reports.
- Processing Reports can be accessed in two different ways.
- Via Invoice > Claim>Click on Show request History > Click on the Request ID in the Medicare Online Request History session.
- Via Invoice > Click on the Hyperlink Here
2. Payment Report
Payment reports will be available a couple of days after the amount been transferred.
Accessing the Payment Reports
Payment reports can be accessed via the Reconciliations.
From CareRight Dashboard
- Click Reconciliation
- Select Eclipse Remittance Advice
- Three tabs
- Manual - ERA which needs manual allocation
- In Progress - ERA in progress
- Archive - Archived ERA.