Introduction
This article applies to IHC claiming both same day and multi-day stay claiming.
When moving from claiming using HC21 forms to sending claims using ecplise there a few minor differences that will need to be considered.
Setup
The first thing to do is enabled the guarantor for ecplise claiming. [Admin>Accounting>Guarantor] edit the guarantor you want to send claims for and set the "Day Hospital IHC claiming" setting to "Electronic Claiming (Eclipse) Onboarding Mode". This allows you to restrict who can send ecplise claims for this gurantor. Once the claims are accepted and you want to enable all claims to send electronically then set the value to "Electronic Claiming (Eclipse) "

Ensure that the users who will be sending these claims have the role "Can onboard In-hospital Claims (IHC)", this is configured in your user groups.
Sending a Claim
When viewing the invoice there will be a new button called "Eclipse Claim" that can be used to send the claim via eclipse. The existing claim and express claim options will generate a HC21 and should not be used for the invoice you want to send via eclipse whilst on boarding. Once the guarantor setting is changed from onboarding to normal eclipse then you will use express claiming as usual and it will send via eclipse.

This will take you to the "non express" screen, however you should be able to proceed through to send the claim without data entry.


if there are no problems you will receive a success message. These messages follow the same format as all other ecplise claiming in CareRight

If there is a problem it might look like:

Status & Payments
The ongoing status and payments or eclipse IHC claims work the same as IMC claims. Payments appear as ERA's and work the same as pay downs of IMC claims.
Eclipse
Claim Generation
Eclipse claim generation is only supported for Day Surgery. If an admission is for more than one day and the guarantor is configured as "Electronic Claiming (Eclipse)" then a message needs to be displayed to the user on the claim screen that a paper-based claim will be created for this claim.
Currently when you "Prepare" a claim that is marked "Electronic Claiming" a Thelma XML file is created. If the guarantor is set to "Electronic Claiming (Eclipse)" instead the system should generate and send a IHC claim via eclipse. In the case when the guarantor is set to "Electronic Claiming (Eclipse)" the 'prepare" button shall be renamed to "Send to Health fund"
Send Claims via Eclipse to Facilitate Health Fund Onboarding (New v6.63 Feature)
This new feature enables users to send specific individual IHC claims via eclipse instead of HC21 forms. This is used for onboarding of health funds.
Requirements
- Display an invoice that is eligible for IHC;
- User belongs to a group with the Can onboard In-hospital Claims (IHC) privilege enabled (done by System Administrator); and,
- For guarantors, in the Day Hospital IHC claiming field, the option Electronic Claiming (Eclipse) Onboarding Mode is selected.


Notes on Requirements
When the Can onboard In-hospital Claims (IHC) privilege is set, the system operates the same as if the mode was set to "Paper Based" for all existing functionality.
Express claiming always uses Paper Based claim when the mode is set to Electronic Claiming (Eclipse) Onboarding Mode.
Functionality
If all 3 of the above requirements are met, then the Eclipse Claim button will appear adjacent to the Claim button. This can be used to generate an Eclipse claim instead of a paper-based claim.

Reallocating an ERA Receipt (New v6.65 Feature)
This feature enables users to reallocate an ERA receipt to an invoice.
- Navigate to Eclipse Remittance Advice screen.
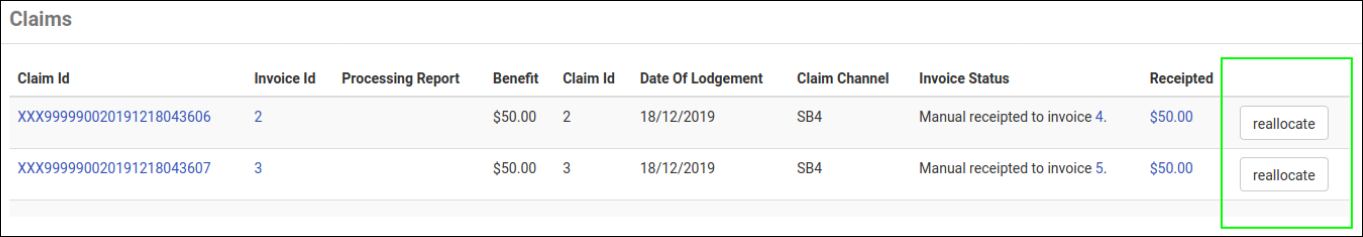
- In the Claims panel, if a receipt is present, it can be reallocated to an invoice by clicking Reallocate.
- The Reallocate Eclipse Remittance Advice screen appears.
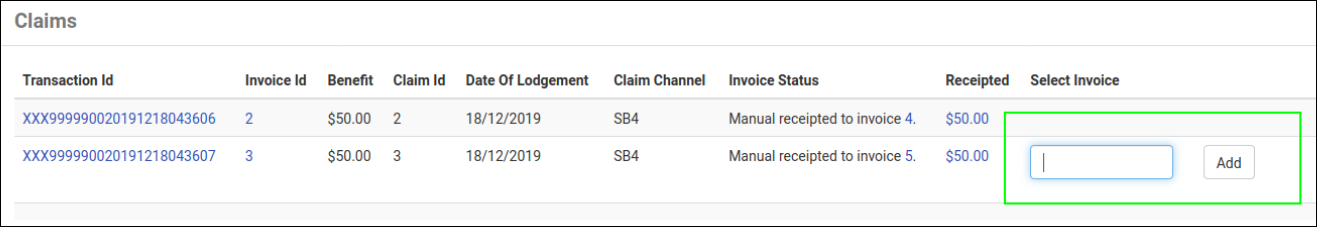
- In the Select Invoice column, select an invoice and click Add.
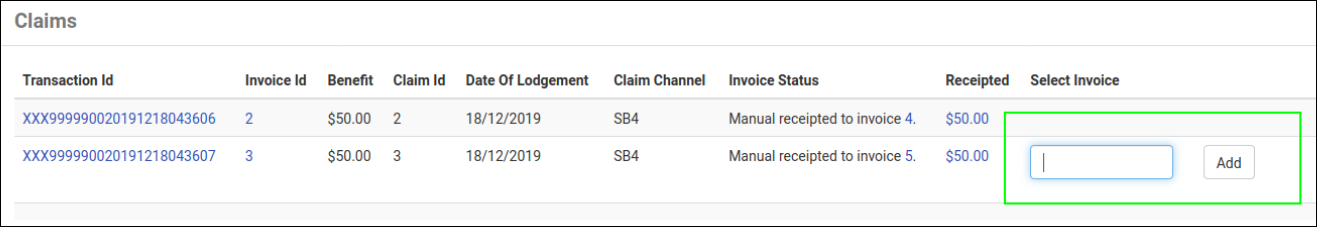
- The invoice's details appear below.
- In the Allocate column, enter the full amount of the receipt to the selected invoice.
- After doing this, CareRight will:
- Reverse the allocation of the statement receipt;
- Remove any associated payment logs for the receipt; and,
- Allocate the statement to the user-specified allocation.
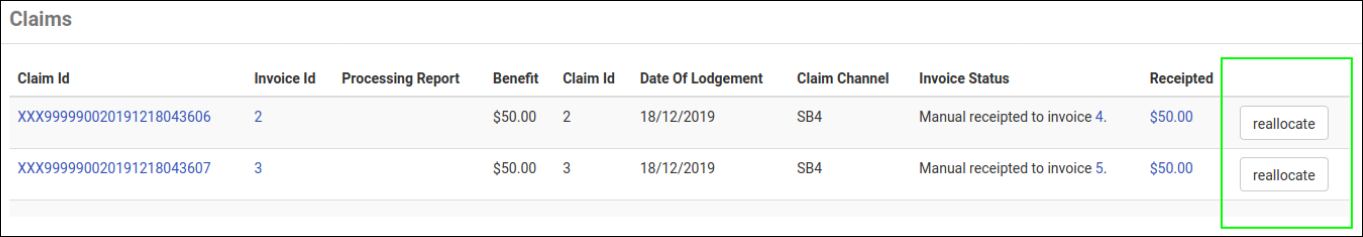
- The Eclipse Remittance Advice screen re-appears.
- Note that the Invoice Status column now includes a link to the receipted invoice number.
Claim Status
Once the claim has been successfully sent to the health fund by eclipse the claim screen will show the status as per the methods outlined by the Medicare communications. The Submissions section is not used or displayed for eclipse claims.
IHC Adjustment Claims
After a successful claim is complete it may be necessary to send an adjustment to the claims. This may be an alteration to the charges of the claim or simply altering other parts of the claim data.
Invoice Adjustments
Claims need to reflect invoice value including adjustments. Currently the claim displays, and uses, the line items values as the per the originally entered invoice value. This needs to be changed to use the value with all adjustments applied.
When building a claim, the adjusted value needs to be used for each segment.
Supplementary Claims
Supplementary claims are extra claims created against an Admission that only contain Miscellaneous or Prosthetic items. (No accommodation or theatre). These are used to claim for extra items after a "normal" claim has been submitted.
When generating a claim and the user selects contiguous claim code of "not in series", the claim has NO accommodation and all items are classified as "Miscellaneous" then the generated claim needs to default to a supplementary claim.
Important Note: There are a number of key setup items for In Hospital Claiming (Eclipse) - please refer to your Systems Administration Guide.
Thelma
To process a claim via Thelma:
- Select Associate that is a service location and click ‘Create Invoice’.
- Select referral or Invoice Override Code.
- Select Service Location and if necessary set invoice date (it will be today’s date by default).
- As Service Location is an Inpatient or Procedure Centre location type then a ‘Default Hospital Settings’ section appears. These should have the correct values by default (which for most funds are the values “Agreements’ and ‘Verbal’ but for Medibank Private are ‘Scheme’ and ‘Not Obtained’).
- Select required completed admission.
- Click Create Invoice.
- Entering line items - For each item on the invoice.
- Set the ‘Date of Service’ if the item wasn’t given/performed today and you failed to set the invoice date above.
- Enter the item number (or select from pop-up list).
- Enter the time the item was given/performed.