In Hospital Claiming (Eclipse) - Day Hospital
Note: Please confirm the mandatory configurations are done correctly in CareRight for the successful handling of IHC Claim via Eclipse. Refer to Configurations for the IHC Claim in the system admin guide for more information. |
Generate an IHC Eclipse Claim
From the invoice eligible for IHC Claim
- Click on the Claim Button
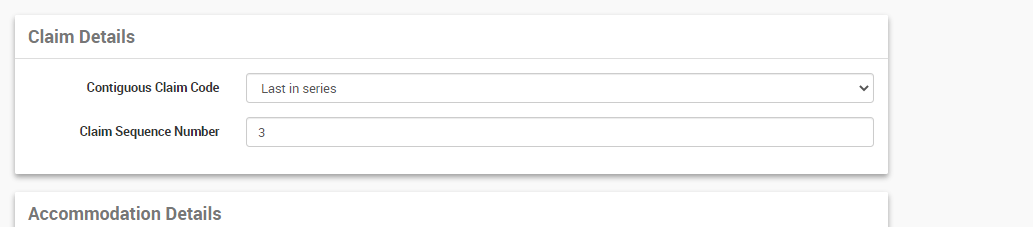
- The next tab will take information on the series levels the claim is submitting for and the sequence number if supplementary claims are submitting as part of the same admission.
- Eg: If multiple Claims are submitting as part of admission, each claim can be assigned with series levels. Clients can claim multiple invoices associated with an admission together or they can be sent individually. If sending individually, the user has to select the Contiguous Claim Code manually as;
- Not in series - If the claim is not part of a series of claims associated with the admission
- First in series - If it is the first claim for the admission and more claims to come on.
- Middle of series - any claims between first and last claims in an admission.
- Last in Series - If it is the last claim in the series for the admission.
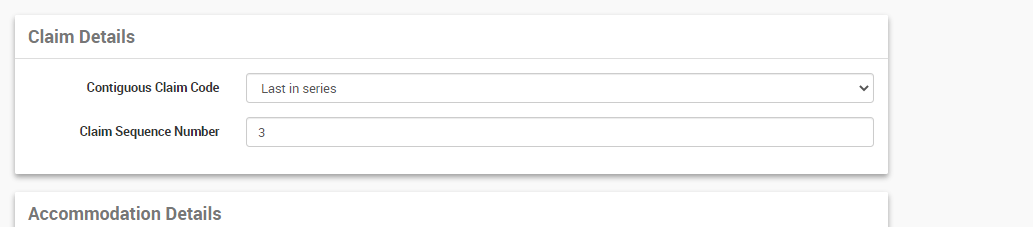
- The Claim Sequence Code will automatically be selected by the system.
- Eg: If multiple Claims are submitting as part of admission, each claim can be assigned with series levels. Clients can claim multiple invoices associated with an admission together or they can be sent individually. If sending individually, the user has to select the Contiguous Claim Code manually as;
- Click Next
- Review the information, Ensure all mandatory fields are filled.
- Any additional notes can be entered in the Remark text area, this will transfer as part of the claim.
- Click Submit
Once the claim has been successfully sent to the health fund by eclipse the claim screen will show the status as per the methods outlined by the Medicare communications in the Medicare Online Request History section.
Please Note: An HC21 Form will be generated instead of the medicare response if the health fund is not configured for Eclipse claiming or claiming for multiday admissions.