What is Changing?
The legacy technology used by CareRight to communicate to Medicare known as the "Medicare Client Adaptor" is being decommissioned by Services Australia. A replacement technology based on modern web services is available in CareRight 6.78. More information is available from Services Australia at: https://servicesaustralia.gov.au/hpwebservices
This technology is used by all CareRight functions which communicate online to Medicare, or to a health fund via Medicare, including:
- Online Patient Verification (OPV)
- Online claims: Bulk Bill, DVA, Patient Claim Interactive (PCI)
In addition, ECLIPSE functions which communicate to health funds via Medicare are also affected:
- Online Eligibility Check (OEC)
- Online claims: Inpatient Medical Claims (IMC), Inpatient Hospital Claims (IHC)
It does not affect off-line (paper) claims, or claims submitted through Thelma.
Do I have to Upgrade?
YES - If you use any of the affected functions listed above, you must upgrade by 13th March 2022.
If you have not upgraded by that date, all online Medicare functions in CareRight will fail.
What do I Have to Do?
Step 1 - Register your Organisation with PRODA
This step can be performed in advance of web services and is available in CareRight 6.75 or later.
Replacing the PKI certificates used by the adaptor, PRODA is an online verification and authentication system managed by Services Australia. You must register your organisation with PRODA and then authorise CareRight via PRODA.
- For information about PRODA see: https://www.servicesaustralia.gov.au/proda-provider-digital-access
Step 1a - Register as an Individual with PRODA
One or more staff need to register as individuals with PRODA before registering the organisation, if they haven't already. At least one of the individuals must be an associate or authorised contact for the organisation according to the Australian Business Register (ABR).
- For guidance on registering as an individual: https://www.servicesaustralia.gov.au/how-to-register-for-individual-proda-account
Step 1b - Register your Organisation with PRODA
An individual (who is an associate or authorised contact on the ABR) can register the organisation in PRODA.
After registering the organisation, the authorised contact may delegate management of the organisation to other individual PRODA accounts. To manage CareRight in PRODA, delegate the role "Device-Management" to another individual. This is optional but recommended so that multiple people are able to manage the CareRight connection to PRODA.
- For guidance on registering an organisation: https://www.servicesaustralia.gov.au/how-to-register-organisation-proda
- For guidance on delegating access to another individual: https://www.servicesaustralia.gov.au/managing-members-and-delegations-organisation-proda
Step 1c - Link your Organisation to Medicare
After registering your organisation, you should add Medicare online as a Service provider to either the Parent Organisation or Sub Organisation, then link to the channel using your existing Minor ID(s).
- To find your existing Minor IDs in CareRight, where they are also labelled as "Location IDs":
- The "Default Location ID (Minor ID)" is shown at: Administration > Accounting > Main Choices > Medicare
- It will start with "CLL0". Do not use the "OEC Location ID" which starts with "CLL9".
- Each service location may have a "Medicare Location ID" shown at: Administration > Locations > Service Locations > Name > Billing
- The "Default Location ID (Minor ID)" is shown at: Administration > Accounting > Main Choices > Medicare
- For guidance on linking Medicare Online to your PRODA organisation: https://www.servicesaustralia.gov.au/adding-and-linking-to-medicare-online-proda
Step 2 - Authenticate CareRight with PRODA
This step can be performed in advance of web services and is available in CareRight 6.75 or later.
You can authorise CareRight to connect to Medicare by adding it as a "B2B Device" in PRODA.
Instructions for this are in the CareRight manual: https://careright.knowledgeowl.com/help/proda-configuration
Step 3 - Upgrade CareRight to at least 6.78
Arrange for an upgrade with Clintel if you are not already running version 6.78. This is the first version which is certified by Services Australia for use with web services.
Step 4 - Cut-over to Web Services
Arrange a time with Clintel to reconfigure your CareRight instance to stop using the adaptor and start using Web Services. This change requires a redeployment causing a 1-2 minute outage.
It would be best to have some online claims ready to send after the cut-over as a test to ensure PRODA authentication and web services configuration is all correct.
Clintel also recommends performing a "Get Participants Request" to test connectivity and also update information about health funds. The instructions for doing this are in the system administrators manual: https://careright.knowledgeowl.com/help/medicare-participants
What User Facing Changes are there to CareRight?
The change is mostly back-end without visible changes that users would notice, or require them to adjust their work-flow. For sending claims, users should simply follow the same steps that they currently do.
Some minor changes are listed below:
General - Error Codes and Messages
In some situations, Medicare may return different error codes or messages than what you are used to. If the meaning of the errors is unclear, contact Clintel or Services Australia for advice.
When viewing a claim that has been sent, there are changes to the layout and sometimes formatting of the data that is sent, due to changes in the underlying data structures. When errors can be correlated with specific parts of a claim, the error will be shown inline.
Online Patient Verification (OPV)
Patient sex is a required field when performing an OPV. If you have a custom assessment that includes an OPV check and does not include the patient field "gender" you will need to make a new version of the assessment. Otherwise you will get a 9202 error during verification.
Online batches (Bulk Bill and DVA)
No changes.
Patient Claim Interactive (PCI)
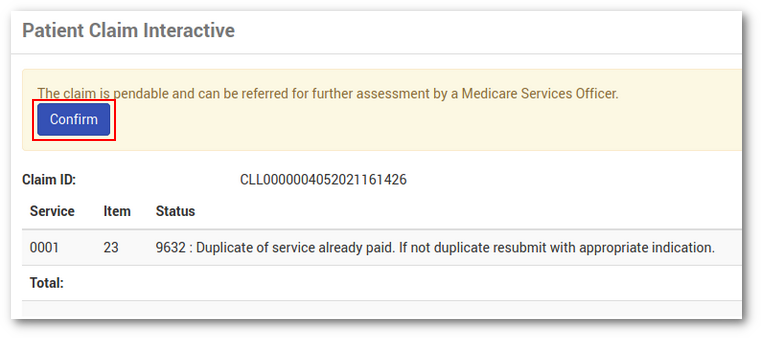
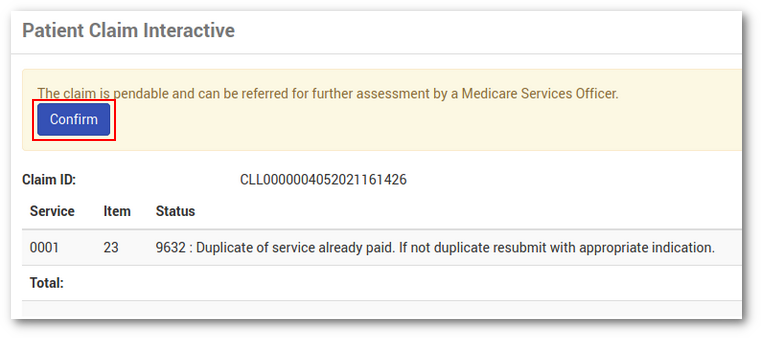
Previously, when a claim had to be referred to a Medicare customer service officer for further assessment, CareRight required the user to resubmit the claim and click the check-box "Automatically Accept Claim":
 This check-box is no longer available. Instead, if the claim can be referred, a new button on the result screen allows this claim to be immediately referred for further assessment:
This check-box is no longer available. Instead, if the claim can be referred, a new button on the result screen allows this claim to be immediately referred for further assessment:
 Statement of Benefit and Claim and Lodgement Advice Form
Statement of Benefit and Claim and Lodgement Advice Form
There are minor wording changes to these printed forms to comply with the most recent Services Australia requirements.
Same Day Delete (SDD)
No changes.
Inpatient Medical Claim (IMC)
No changes.
Inpatient Hospital Claim (IHC)
Default codes sent via IHC will now use the most recent version of HCP coding. For example:
- "Acute Care" previously mapped to "10", now it maps to "1" in the claim
- "Rehabilitation" previously mapped to "20", now it maps to "2" in the claim
ECLIPSE Remittance Advice (ERA)
No changes - CareRight will continue to retrieve these automatically.
Online Eligibility Check (OEC)
There are minor wording changes to the on-screen and printed OEC declaration to comply with the most recent Services Australia requirements.
Get Participants Report (GPR)
Additional information is available to the system administrator when viewing a health fund guarantor; The Medicare Participant now lists the online functions that the guarantor is allowed to receive. This is for information only, it does not prevent a user from trying to send a claim to a health fund which doesn't support it.
Frequently Asked Questions
As web services is rolled out to CareRight customers, any common issues or problems will be added here.
 Statement of Benefit and Claim and Lodgement Advice Form
Statement of Benefit and Claim and Lodgement Advice Form