CareRight automatically checks on the status of all outstanding claims daily at:-
- 8 AM for Medicare & DVA bulk bill batch claims
- 7 AM and 3 PM for IMC & IHC (same day) claims
Where those claims are paid in the amount claimed, receipts/payments will automatically be raised on the relevant patient accounts and the claims will be marked as paid.
If the claim is not paid in the amount claimed (paid a different amount or not paid at all) then the claim will be marked as a problem.
An overview of the outstanding claims can be seen in the 'Invoices & Claims' window

By clicking on any of the blue numbers you can see a list of the invoices in that status

Once we know which invoices are a problem, we need to find out what the problem is. Depending on what the problem is, we may have to:-
- Modify the invoice and re-submit the claim
- Cancel the invoice and raise a replacement invoice with the required changes
- Raise an adjustment for the difference between the billed and paid amounts
- Write off the claim
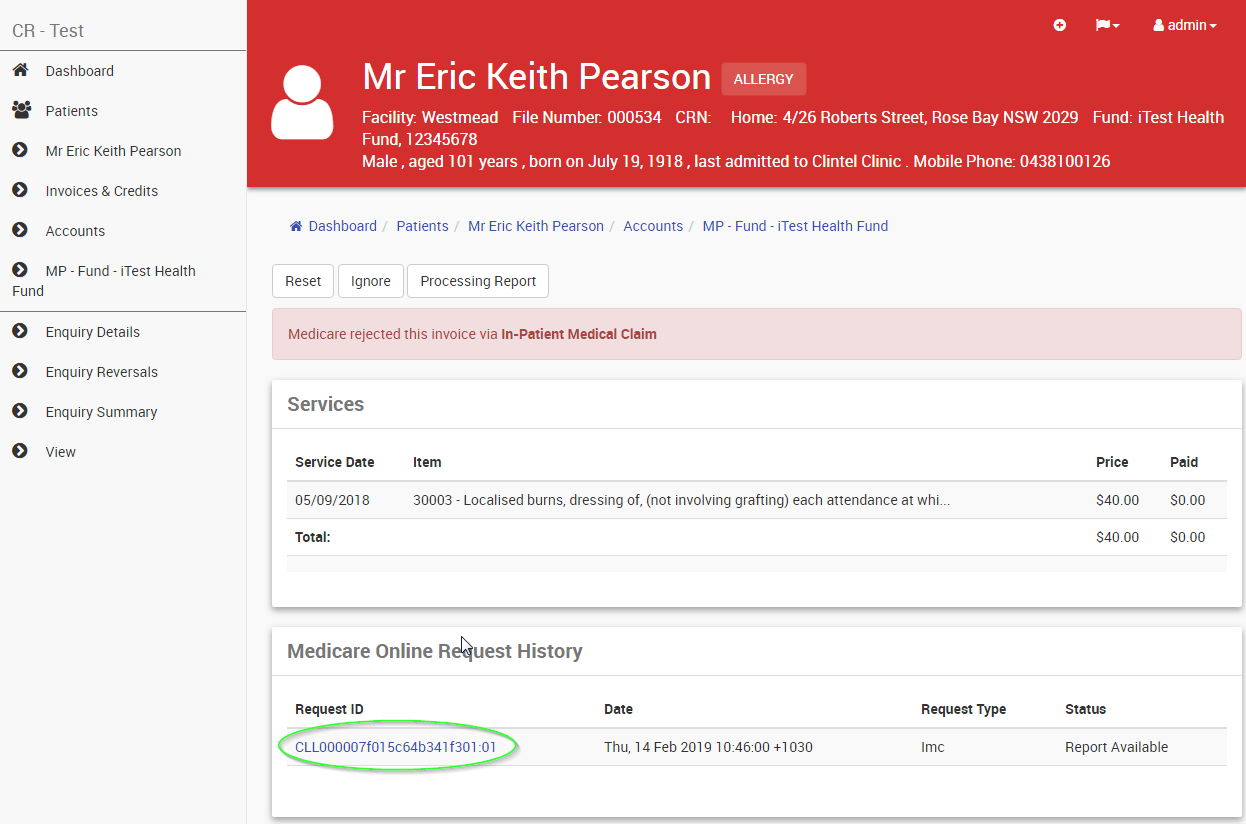
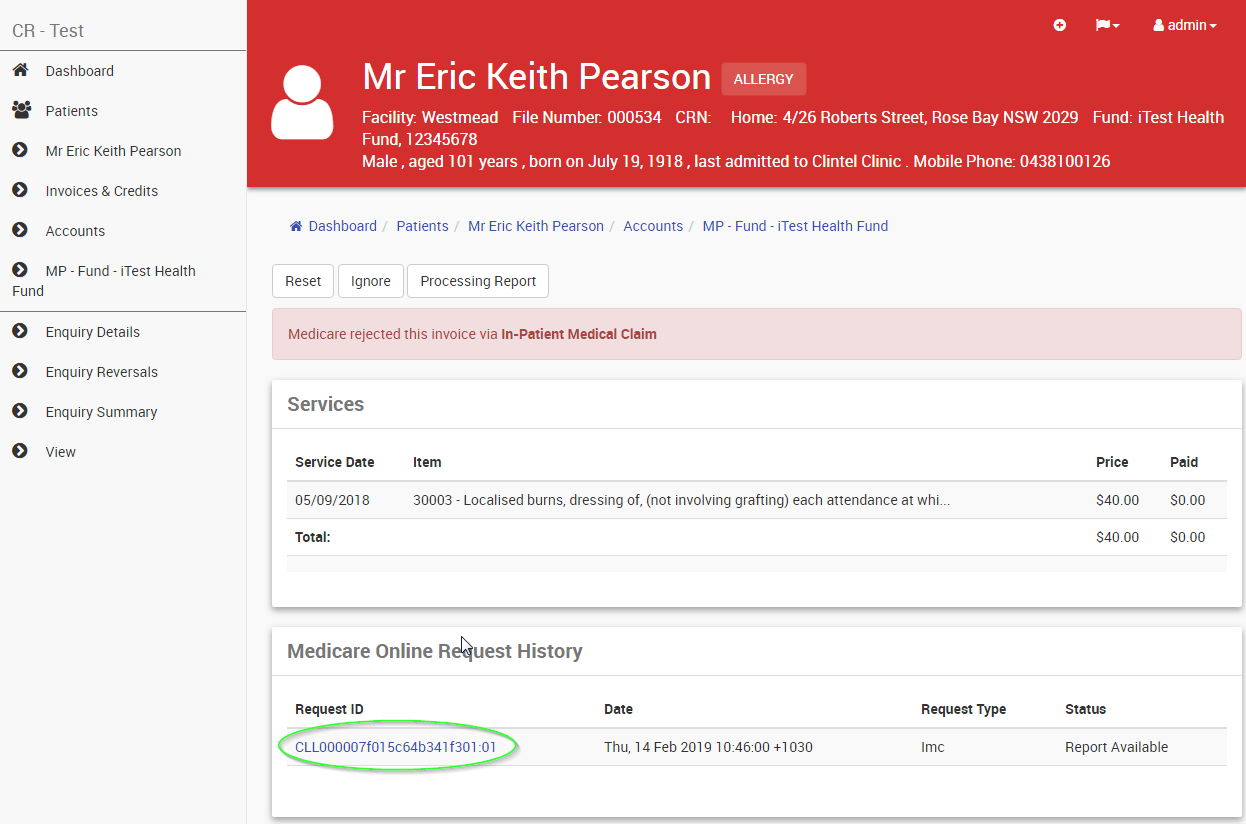
To identify why an invoice has been marked as 'Problem'
From the window with the list of problem invoices for a given provider
- Open the invoice by clicking on the invoice number hyperlink
- Click the Claim button just below the banner (for Medicare and DVA click the 'Batch Claim' button and skip to step 5)
- Click the Show Request History button
- Click link for the most recent submission of the claim
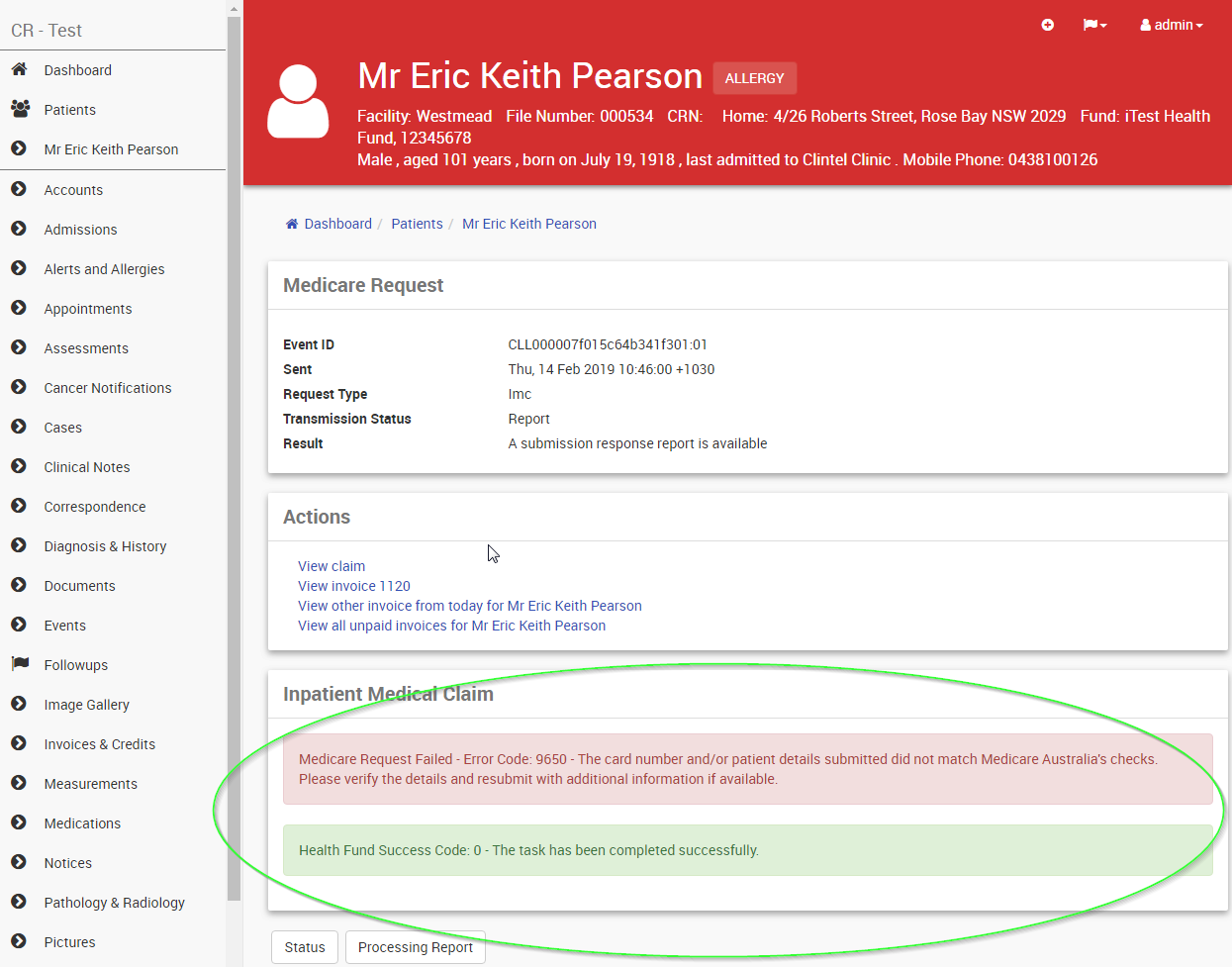
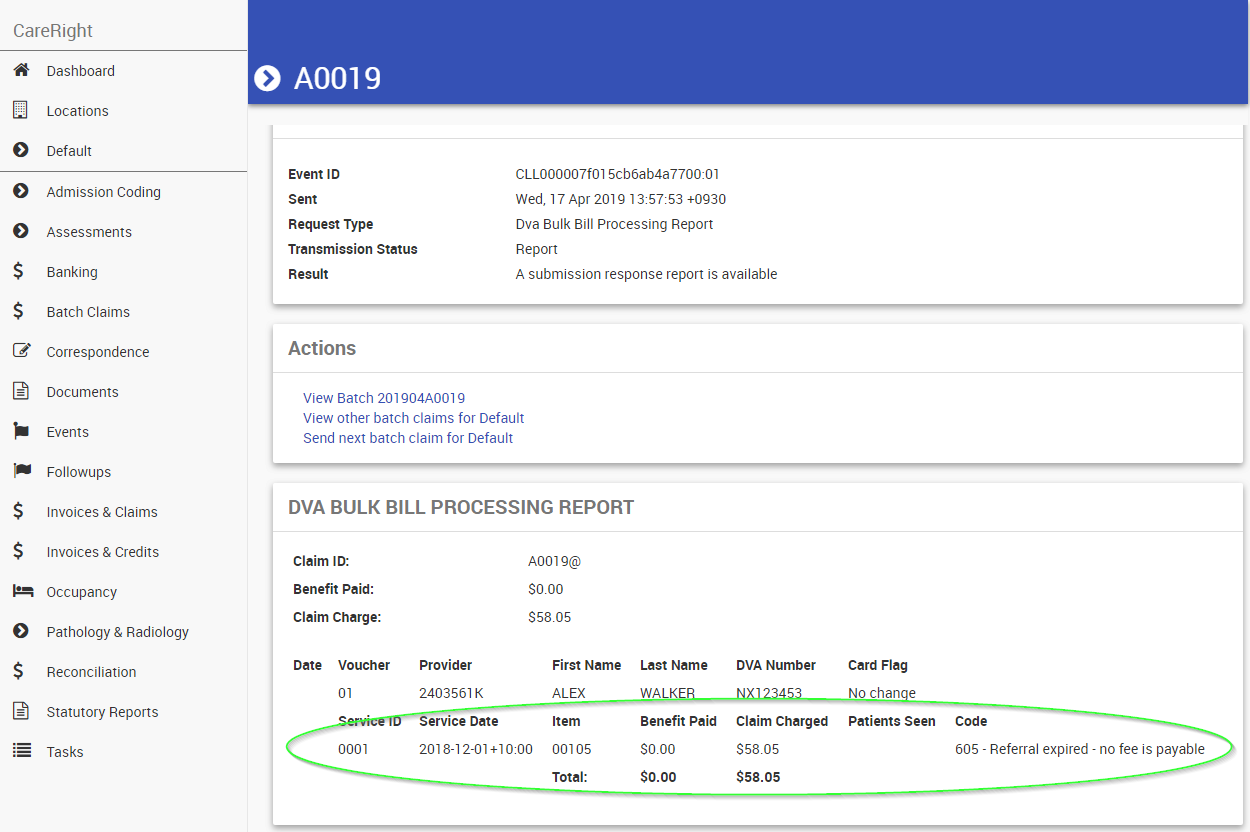
- After the 'Actions' section there may be displayed any warning messages about why the claim failed
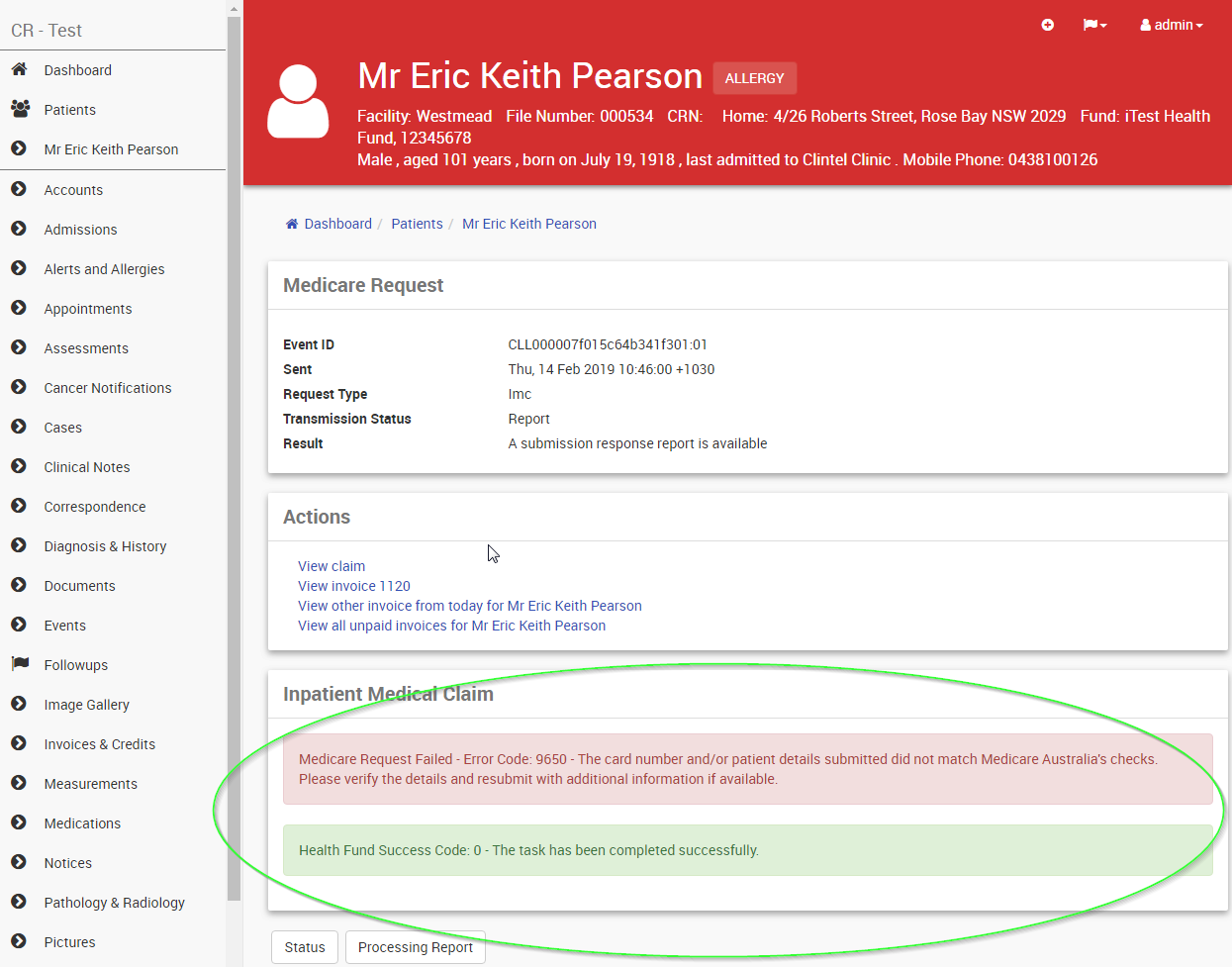
The codes and descriptions for the rejections codes come directly from Medicare. The list can be accessed at
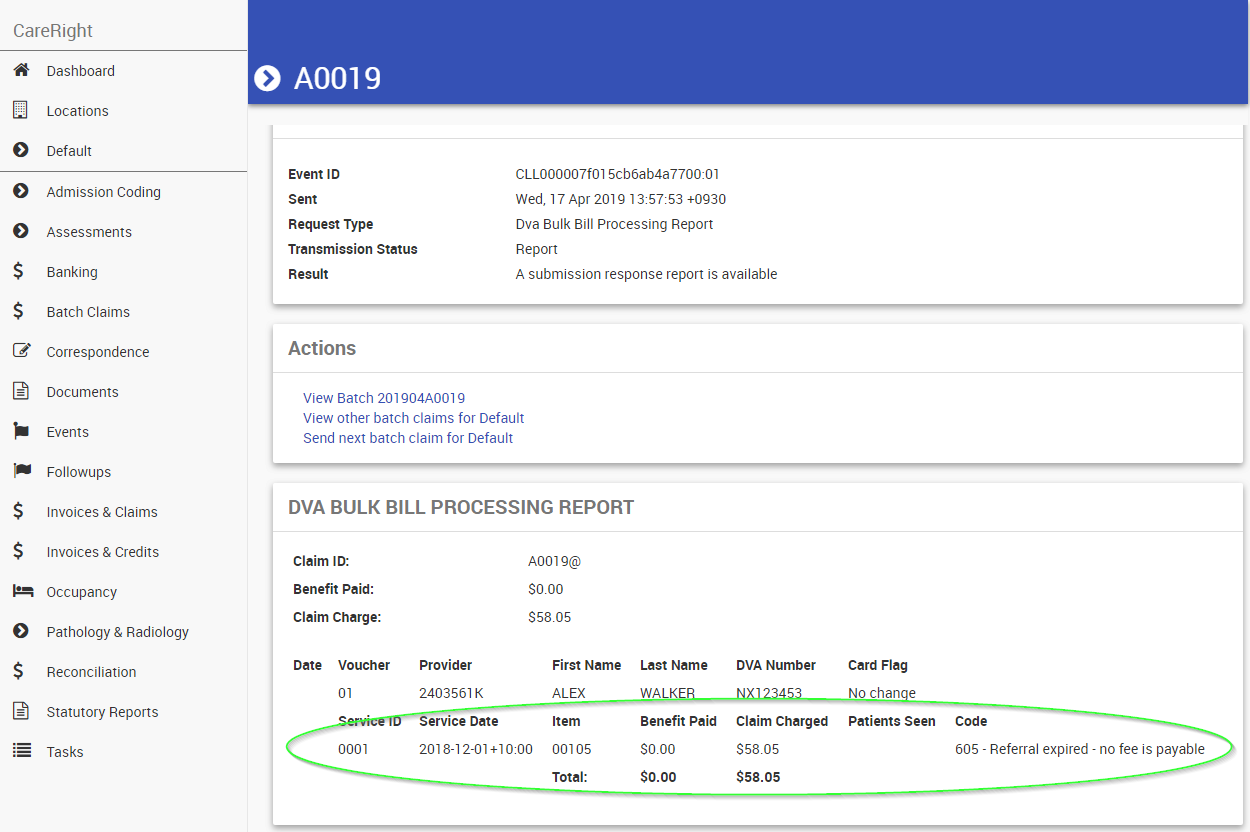
https://www.humanservices.gov.au/organisations/health-professionals/services/medicare/simplified-billing-and-eclipse/managing/medicare-digital-claiming-return-codes - Look for the most recent 'Processing Report' in the list of reports at the bottom of the screen and open it
- If no 'Processing Report' is present, click the Processing Report button
- The Processing report will detail the reasons that any item was not paid at the claimed amount.
Reconciling Medicare Batch Payments
Navigating to Invoices & Claims > Manual Batch Payments will allow you to reconcile Medicare / DVA batch Payments
There are 3 tabs at the top of the screen these are:
Manual - need to manually allocate due to reversed invoices, invoices removed from the batch or payments that are older that 10 days old that have been unable to have automatic allocations done.
In Progress - These are batched payments that have reported but are waiting on a Medicare or dva processing report to allocate money to individual line items
Archived - These are payments that have been fully reconciled

If a payment is waiting in the manual tab users will need to manually allocate a portion of the money to items. Clicking Show on any on of these followed by Allocate button to will allow them to allocate any money that has not been automatically applied to invoice items. In the case displayed below batch A0007@ has been automatically allocated but batch A0008@ requires manual allocation of funds.
Users will be presented with a list of invoices in batch that have not had allocations made to them but have a payment that needs to be allocated. Users must select an invoice to allocate to before clicking the Add button. In the case displayed below Medicare have paid $66.30 and the batch have 2 invoices. In this case both invoices total the payment amount but in some cases this will not be the case as medicare may reject some invoices of pay differing amounts due to other medicare rules. If the Invoice has been reversed, already paid or been removed from the batch the use has the ability to:
- allocate to the invoice listed by adding the same invoice id
- allocate to a new invoice number that has been created to reconcile the payment received.

Once all invoices have a replacement invoice number then the payment must be allocated to to the invoice items. NOTE: leaving an allocation of $0 is ok but this screen will not allow users to save the payment until the total Payment amount has been allocated to invoice items. In the case shown bellow invoice 16 has had $36.55 allocated to it and invoice 17 has had $29.75 allocated to it. Once money has been allocated clicking the Allocate button will allocate the money to line items.
If allocations all total correctly and are saved to Careright then the batch payment will be moved to the Archived section of payments. NOTE: User will be directed back to the Manual page ready to manually allocate the next payment. But if the user searches for the payment in the Archived section and clicks show then they will be able to see the allocations that were manually made.
Reconciling Health Fund (ERA) Payments
Navigating to Invoices & Claims > Manual ERA Payments will allow you to reconcile any healthfund payments for IHC or IMC claims

There are 3 tabs at the top of the screen these are:
Manual - need to manually allocate due to reversed invoices or payments that are older that 10 days old that have been unable to have automatic allocations done.
In Progress - These are payments that have reported but are waiting on a processing report to allocate money to individual line items
Archived - These are payments that have been fully reconciled

Standard Allocation
If a payment is waiting in the manual tab users will need to manually allocate a portion of the money to items. Clicking Show on any on of these followed by Allocate button to will allow them to allocate any money that has not been automatically applied to invoice items. In the case displayed below batch 2 invoices have require allocation as a processing report has not been able to allocate funds automatically within 10 days of receiving the payment.
Users will be presented with a list of invoices that have not had allocations made to them but have a payment that needs to be allocated. Users must select an invoice to allocate to before clicking the Add button. In the case displayed below the Fund has paid $50 to a single invoice. In this case the benefit equals the payment amount but in some cases this will not be the case due to patient co payments, excesses or payment may differ due to fund rulings. If the Invoice has been reversed, already paid the user will need to allocate to a new invoice. In the case shown below an invoice 50 has been created to receive the money that paid for invoice 40.

Once all invoices have a replacement invoice number then each payment must be allocated to to the invoice items. NOTE: leaving an allocation of $0 is ok but this screen will not allow users to save the payment until the Payment amount has been allocated to invoice items. In the case shown bellow invoice 50 requires $50 allocated to it. Once all invoices have been allocated clicking the Allocate button will allocate individual receipts to each invoice manually allocated to.
If allocations all total correctly and are saved to Careright then the ERA payment will be moved to the Archived section of payments. NOTE: User will be directed back to the Manual ERA page ready to manually allocate the next payment. But if the user searches for the payment in the Archived section and clicks show then they will be able to see the allocations that were manually made.
Reallocate Payment
Sometimes money automatically or manually allocated needs to be reallocated to a different invoice. Searching for the payment in the Archived and clicking show will then present the user with a reallocate button. NOTE: clicking the Reallocate button will only relocate the individual invoice within the payment. If multiple invoices require reallocation then each change must be done separately. The user must firstly pick a replacement invoice to allocate to.

Once the invoice have a replacement invoice number then the payment must be allocated to the invoice items. NOTE: leaving an allocation of $0 is ok but this screen will not allow users to save the payment until the Payment amount has been allocated to invoice items. In the case shown bellow invoice 51 requires $50 allocated to it. Once all invoices have been allocated clicking the Reallocate button will update the allocations to the new invoice.
Over / Under payment
There are times when Funds will pay under or over the amount shown on the ERA. Medicare or the Fund will supply you with a formal paper document detailing why they have under overpaid. This is usually done if a old invoice with a derived item has been reassessed. These payments will always be show in the Manual ERA section as there is no electronic way of matching these reassessed payments to invoice services. In the example below the fund has paid $60 but report only details $50 of payments. Clicking the Allocate button will allow users to manually allocate this additional money

Users will be presented with an Unallocated section listing a positive or negative value of money that need to be allocated.
User must add an:
- Invoice number
- An arbitrary amount
This will then add a section allowing the arbitrary amount to be allocated to the invoice. NOTE: The Unallocated section will continue to show until all the credit / debit has been accounted for. In the example below I will allocate $5 to invoice 53 and $5 to invoice $54.

Once each of the arbitrary amounts to be allocated to the invoice then clicking Allocate will create receipts / refunds for the funds. In the example below I have created 2 arbitrary amounts
- $5 must be allocated to invoice 53
- $5 must be allocated to invoice 54
Once each invoice has had the Payment amount allocated to it and the Allocate button has been clicked the receipt or refund is created accounting for these under / over payments.

If allocations all total correctly and are saved to Careright then the ERA payment will be moved to the Archived section of payments. NOTE: User will be directed back to the Manual ERA page ready to manually allocate the next payment. But if the user searches for the payment in the Archived section and clicks show then they will be able to see the allocations that were manually made.